14/11/2022
The team of Gilles Crambert and Pascal Houillier, Renal Physiology and tubulopathies, recently published in JASN a singular story, revealing a novel chain of causality in an unusual renal pathology, and allowing to propose an adapted treatment.
The story is that of a patient admitted to the hospital because of severe tetany with renal failure. Examinations showed massive and selective loss of calcium and magnesium in the urine, suggestive of familial hypomagnesemia syndrome, a genetic disease of autosomal recessive transmission. It is caused by mutations in the genes coding for Claudin 16 or Claudin 19, CLDN16 or CLDN19, tight junction proteins specifically expressed in a particular segment of the renal tubule, the large ascending branch of the loop of Henle.
However, some elements of the picture seem inconsistent with the existence of this syndrome. Familial hypomagnesemia usually reveals itself in childhood, but the patient was 70 years old. In addition, analyses performed 2 years earlier did not show any loss of calcium and magnesium in the urine; finally, the CLDN16 and CLDN19 genes were perfectly normal.
The researchers therefore hypothesized a “phenocopy” of familial hypomagnesemia, i.e., a disease with the same signs as this disease, but linked to an acquired rather than a genetic cause. A series of in vitro and in vivo experiments in rodents showed that the patient’s plasma did indeed contain a high titer of anti-Claudine 16 antibodies and that these antibodies were pathogenic in rodents.
Treatment with an immunosuppressant, Rituximab, and plasma exchange to eliminate the circulating pathogenic antibodies resulted in improvement in renal function and renal calcium loss syndrome.
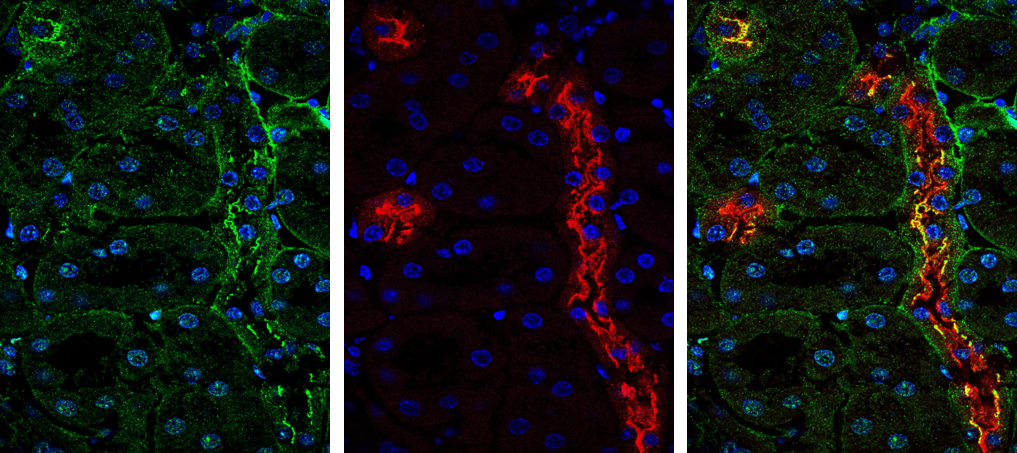
However, several months after this episode, the patient’s general condition deteriorated again, with deterioration of renal function and worsening of calcium and magnesium loss in the urine. A new abdominal CT scan revealed a large, poorly differentiated renal tumor with high expression of the CLDN16 gene. Removal of the tumor kidney allowed to stabilize the renal function and to normalize the plasma magnesium concentration.
Conclusion: the pathology initially identified, a “phenocopy” of familial hypomagnesia, only revealed another pathology not yet detected, the renal tumor.
Thus, behind a syndrome mimicking a genetic disease, one can find an autoantibody (1st hidden pathology), and behind the expression of an autoantibody, one can discover a tumor (2nd hidden pathology) which expresses a protein in an immunizing way, here Claudine 16.
The organism does not start to produce an autoantibody by chance: looking for the immunizing protein can lead to the discovery of a cancer.
Hypomagnesemia, Hypocalcemia, and Tubulointerstitial Nephropathy Caused by Claudin-16 Autoantibodies. Figueres L, Bruneau S, Prot-Bertoye C, Brideau G, Néel M, Griveau C, Cheval L, Bignon Y, Dimitrov J, Dejoie T, Ville S, Kandel-Aznar C, Moreau A, Houillier P, Fakhouri F. J Am Soc Nephrol. 2022 Jul;33(7):1402-1410. doi: 10.1681/ASN.2022010060
Contact
Pascal Houillier, Deputy Director of the Renal Physiology and tubulopathies team

