*Chronic lymphocytic leukemia (CLL), the most common form of chronic leukemia in Western countries, is characterized by clonal proliferation and the accumulation of mature CD5+CD23+ B lymphocytes in the bone marrow, peripheral blood and lymphoid tissues. CLL is biologically and clinically a very heterogeneous disease, where some patients never require therapy and others display an aggressive course with poor response to therapy and death within months. CLL can evolve into an aggressive lymphoma known as Richter’s syndrome, in 2 to 9% of patients and up to 20% of refractory cases. Until recent years, treatment was mainly based on immunochemotherapy: combination of fludarabine, cyclophosphamide and the anti-CD20 antibody rituximab (FCR) or bendamustine-rituximab. The introduction and approval of novel molecularly targeted drugs have provided additional treatment options for patients with CLL. Among them, Bruton Tyrosine Kinase inhibitors (BTKi), which repress B-cell receptor (BCR) signaling, and the anti-apoptotic BCL-2 protein antagonists, such as venetoclax, are the most widely used targeted drugs. These novel agents have demonstrated important clinical efficacy, including in high-risk patients. However, despite these recent therapeutic advances, CLL remains an incurable disease, with relapses and patients developing drug-resistance. Thus, the search for new therapeutic opportunities remains a topical issue. Our team is contributing to this challenge by gaining a better understanding of the pathophysiology of this disease through three complementary approaches:
(i) – Aggressive forms of CLL (F Nguyen-Khac, E Chapiro).
Our team continues to study in depth three still little explored chromosomal abnormalities associated with aggressiveness, poor prognosis and resistance to targeted anti-CLL therapies (e.g. BTKi): (1) gain of the short (p) arm of chromosome 2 (Kostopoulou et al., Cancer Med. 2019; Cosson et al., Leukemia 2017; Chapiro et al., Leuk Res. 2010); (2) 8p deletion (Jondreville et al., Leukemia 2023) and (3) MYC aberrations (translocations and gains; Chapiro et al., Blood 2019). The relevance of these abnormalities in CLL pathophysiology and drug resistance are currently analyzed: (i) in specific cell line models modified by CRISPR/Cas9 that mimic these three aberrations (already present in our laboratory); (ii) in primary CLL cells by analyzing the world’s largest cohorts for each of these three aberrations (TEACLL cohort); and (iii) by comparing the survival and treatment response of patients included in the TEACLL cohort with a control CLL cohort. Cellular and molecular biology techniques, optical genome mapping, transcriptomics, single-cell RNASeq, and bioinformatics approaches are used here.

(ii) Role of the BCR in the pathogenesis of CLL (F Davi, M Armand, C Bravetti).
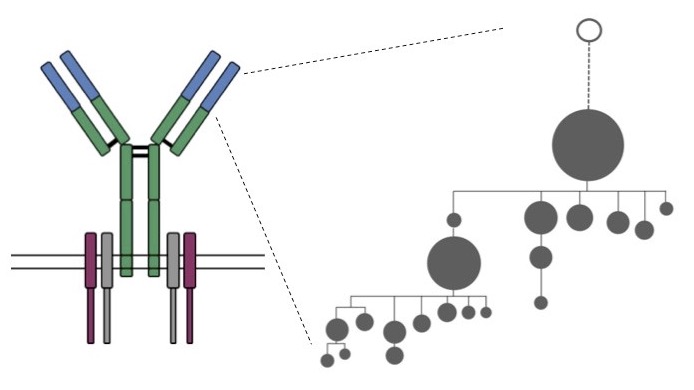
The study of antigen receptors on the surface of lymphocytes, in particular the B cell receptor (BCR), is one of the central themes of our group. On the one hand, the complex genetic recombinations (VDJ rearrangements) required for their formation constitute unique molecular markers for each lymphocyte, which are highly useful for the diagnosis and monitoring of lymphoid tumors. It is also becoming increasingly clear that the BCR plays a critical role in the pathogenesis of many B-cell lymphoproliferative disorders.
Over the last few years, our team has developed methods for analysing BCRs using high throughput sequencing (HTS), within a European collaborative project (EuroClonality) (Langlois de Septenville A et al, Methods Mol Biol. 2022 and Davi F et al, Leukemia. 2020). We now aim to: (i) analyze the light chains genes, as some of them might be of prognostic interest in CLL; (ii) sequence long DNA fragments using Nanopore technology (collaboration with J. Strefford, UK), to detect molecular anomalies downstream of Ig variable regions; (iii) assess the extent and impact of intraclonal diversity in Ig genes on disease evolution and response to treatment. In collaboration with the team of J. Bernardes (Sorbonne University), we have created the ViCloD software package, enabling rapid and easy visualization and analysis of the intraclonal diversity of BCRs resulting from the process of somatic hypermutations (SHM) (Jeusset L et al, NAR Genom Bioinform. 2023). We will continue our efforts to implement this software with new functionalities (molecular characteristics of HMS, longitudinal studies, etc.), some of which will involve artificial intelligence.
(iii) Metabolic reprogramming in CLL (SA Susin, D Garnier).
Studies on cancer cell metabolism have enjoyed a recent renaissance with the recognition of an altered metabolism as a critical component of the tumor phenotype. As a follow, studies on tumor metabolism have received a notable interest in the last years and the analysis of the metabolic reprogramming has uncovered tumor cell vulnerabilities, leading to the development of combined anticancer therapeutic approaches.
(a) Our laboratory has recently shown that fatty acid metabolism fuels mitochondrial OXPHOS in CLL B cells, and that its inhibition leads to mitochondrial alterations and cell death. More precisely, the peroxysomal fatty acid oxidation (pFAO) pathway (a poorly understood metabolic path) seems to play an essential role in fueling mitochondrial OXPHOS in CLL (Tannoury et al. Leukemia, 2023 in press). Following these data, this part of our research program aims to analyze: (i) the pFAO metabolic pathway in a larger panel of CLL B cells, including cells from refractory or relapsed patients; (ii) whether pharmacological modulation of FAO, alone or in combination with anti-CLL drugs, could be used as a therapy to eliminate drug-resistant or relapsed CLL cells; (iii) the specificity of such therapy (e.g., whether metabolic therapy kills tumor cells while sparing non-tumor immune cells); and (iv) the in vivo potential of a pFAO metabolic therapy.
(b) Bidirectional interactions between leukemic B cells and non-transformed cells, including stromal cells, can lead to the establishment of an immunosuppressive microenvironment favoring CLL survival. Recently, the exchange of extracellular vesicles (EVs) has been proposed as a new means of communication (Dubois K et al., Cancers 2023). EVs are composed of exosomes (30 to 150nm) and microparticles (150nm to 1μm), have an impact on physio-pathological processes and contain selective patterns of microRNA, protein or DNA, which can be transferred into target cells. We recently demonstrated that in CLL patient cells, stromal EVs compensate for toxicity induced by blocking glucose entry, suggesting a metabolic reprogramming towards glycolysis. Using metabolomic, fluxomic and transcriptomic + bioinformatic approaches, our aim is now to clarify the modalities of this EV-mediated stromal-CLL cooperation, with particular interest in the hypothesis of an epigenetic regulation.


