15/11/2021
In a recent study published in Diabetes, Francine Béhar-Cohen’s team at the Cordelier Research Center shows that the mineralocorticoid receptor and some of its ligands are overexpressed in the retina of patients with diabetic retinopathy. Intraocular injection of controlled-release spironolactone, which specifically blocks the mineralocorticoid receptor, reduces the early inflammatory response and retinal edema and decreases vascular permeability associated with advanced diabetic retinopathy in rats. These results are a major advance in the understanding of the mechanisms of diabetic retinopathy and constitute a valuable therapeutic lead for the treatment of early and advanced retinopathies.
The worldwide prevalence of diabetes will reach 642 million people by 2040. Diabetic retinopathy is a serious complication of diabetes that affects 50% of type 1 diabetic patients and 30% of type 2 diabetic patients after 10 years. It is the leading cause of blindness before the age of 60. Retinal inflammation, oxidative stress and glial cell dysfunction are recognized as major pathogenic factors in ischemic neuronal damage and macular edema, both of which are responsible for vision loss.
Currently, the main treatments to reduce macular edema are repeated intraocular injections of anti-VEGF or glucocorticoids. Anti-VEGFs neutralize the deleterious effects of members of the VEGF family (increased permeability of the blood-retinal barriers and induction of angiogenesis) while glucocorticoids have an anti-inflammatory and anti-angiogenic role.
However, these treatments are not always effective for all patients, who either do not respond to the treatment, or develop resistance over time, or suffer significant side effects in the case of glucocorticoids. This is why it is important to develop new therapeutic approaches.
Activation of the mineralocorticoid pathway is implicated in diabetes-associated pathologies (heart disease and nephropathy) through, among other things, its pro-inflammatory, pro-oxidant and pro-fibrotic action. Preclinical and clinical studies have shown the beneficial effects of mineralocorticoid receptor (MR) antagonists in reversing proteinuria and slowing the progression of nephropathy in diabetic subjects.
However, the role of MR has never been studied in diabetic retinopathy. Our study published in “Diabetes” showed overexpression of MR in the retina of patients with diabetic retinopathy, and identified cortisol, the endogenous glucocorticoid, as the major ligand for MR in the eye of patients. Lipocalin 2 and galectin 3, which are targets of MR and biomarkers of diabetic complications, were also increased in human diabetic retina. Taken together, these results point to an overactivation of the MR pathway in diabetic retinopathy.
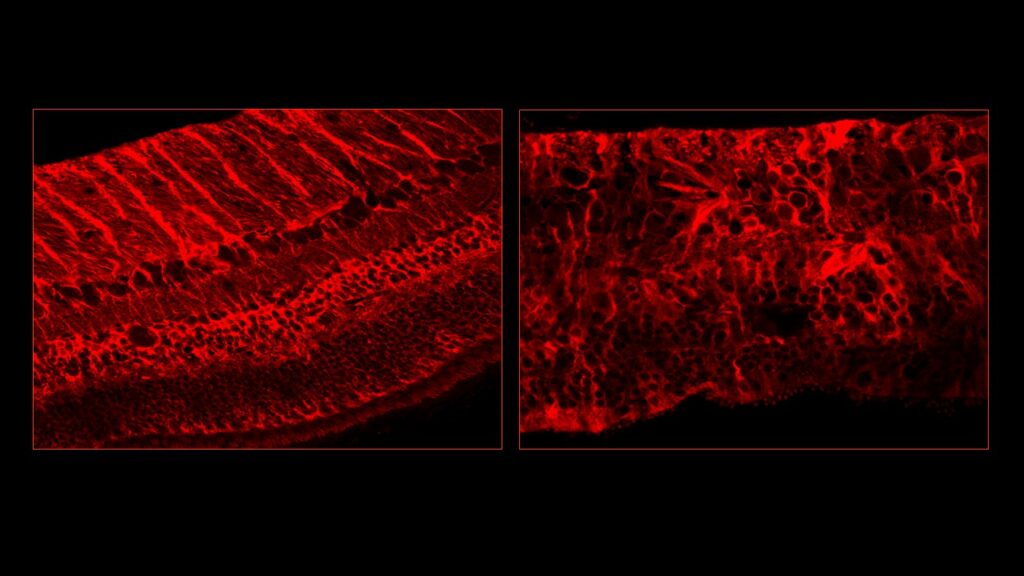
“We tested the effect of controlled intraocular release of spironolactone, a very potent MR antagonist, in Goto-Kakizaki rats, an animal model of type 2 diabetes,” explains Min Zhao. “Our results show that this treatment improves early inflammation, reduces retinal edema and decreases vascular permeability in advanced diabetic retinopathy in rats. Spironolactone would also allow relocalization of ion (Kir4.1) and water (AQP4) channels along retinal Müller glial cells. The transcriptomic study identified genes (e.g., Vldlr, Pten, Slc7a1, Tjp1, Sesn2) and functional groups of genes involved in vascular permeability, blood-retinal barrier, and edema.”
This study is an important advance in understanding the mechanisms of diabetic retinopathy. Blocking the mineralocorticoid receptor, which targets a range of pathological manifestations associated with diabetic retinopathy, represents a new therapeutic avenue with great potential to be explored.
Contacts :
Min Zhao : min.zhao@inserm.fr
Francine Behar-Cohen : francine.behar@gmail.com
Article :
Mineralocorticoid Receptor Pathway and its Antagonism in a Model of Diabetic Retinopathy.
Zhao M, Gelize E, Levy R, Moulin A, Azan F, Berdugo M, Naud MC, Guegan J, Delaunay K, Pussard E, Lassiaz P, Bravo-Osuna I, Herrero-Vanrell R, Behar-Cohen F.
Diabetes. 2021 Aug 23:db210099. doi: 10.2337/db21-0099. Online ahead of print.PMID: 34426510

